The Gut-Brain Connection and Mental Health
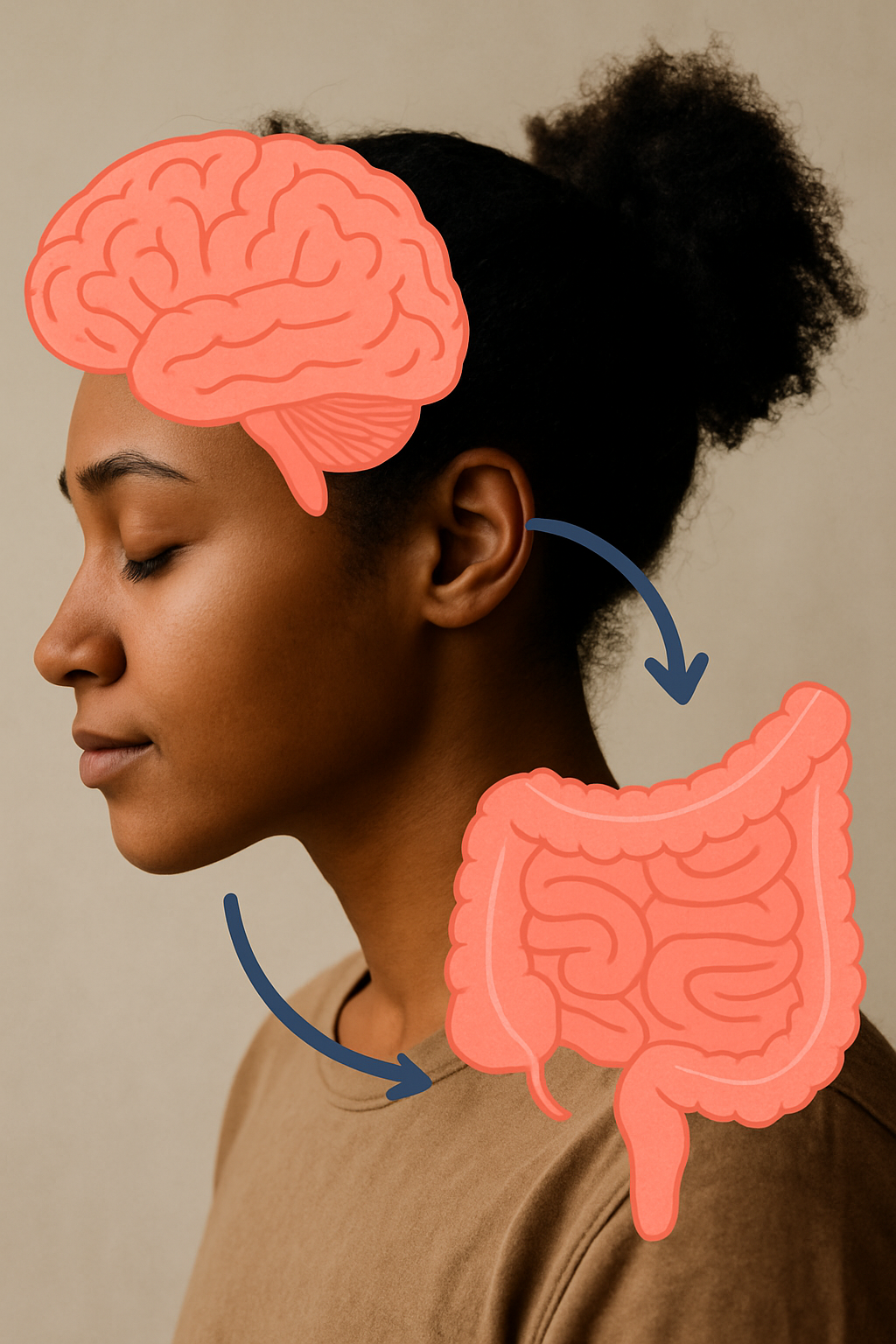
The human gut is often referred to as the "second brain" due to its intricate communication with the central nervous system. This connection, known as the gut-brain axis, plays a critical role in regulating mental health.
Emerging research suggests that the gut microbiome—the diverse community of microorganisms residing in the gastrointestinal (GI) tract—significantly influences mood, cognition, and overall mental well-being.
Understanding the gut-brain connection may provide new strategies for managing mental health conditions such as depression, anxiety, and stress-related disorders.
The Gut-Brain Axis: A Bidirectional Communication System
The gut-brain axis (GBA) is a complex network linking the enteric nervous system (ENS) of the GI tract with the central nervous system (CNS). This bidirectional communication occurs through multiple pathways, including:
Neural Pathways: The vagus nerve acts as a primary channel for transmitting signals between the gut and brain.
Endocrine System: The hypothalamic-pituitary-adrenal (HPA) axis regulates stress responses through the release of cortisol, which can impact gut function.
Immune System: The gut-associated lymphoid tissue (GALT) modulates immune responses, which can influence neuroinflammation and mental health.
Microbial Metabolites: Short-chain fatty acids (SCFAs) and neurotransmitters like serotonin and gamma-aminobutyric acid (GABA) are produced by gut bacteria and play roles in brain function.
Gut Microbiome and Mental Health Disorders
Depression and Anxiety
Several studies have shown that individuals with depression and anxiety often have altered gut microbiota composition. Dysbiosis—an imbalance in gut bacteria—can lead to increased intestinal permeability ("leaky gut"), systemic inflammation, and reduced production of mood-regulating neurotransmitters.
Serotonin Production: Approximately 90% of the body's serotonin, a key neurotransmitter in mood regulation, is produced in the gut.
GABA and Dopamine: Certain gut bacteria, such as Lactobacillus and Bifidobacterium, produce GABA, which has calming effects on the brain.
Stress and the Gut Microbiome
Stress is a disruptor of the gut microbiome according to Registered Dietitian Jessica Martinez of Finch™ Nutrition.
Chronic stress can disrupt the gut microbiota, leading to a decrease in beneficial bacteria and an increase in pro-inflammatory species. The resulting inflammatory response may contribute to cognitive impairment and emotional dysregulation.
Cognitive Function and Neurodegenerative Diseases
Emerging research suggests that gut microbiota imbalances may be linked to neurodegenerative disorders such as Alzheimer’s and Parkinson’s disease. Microbial metabolites like SCFAs have been shown to support neuroprotection, while dysbiosis may accelerate cognitive decline.
Strategies for Supporting Gut and Mental Health
California Registered Dietitian Jessica Martinez of Finch™ Nutrition says a Mediterranean diet is helpful in promoting the gut/brain connection.
Probiotics and Prebiotics: Supplementing with beneficial bacteria (Lactobacillus and Bifidobacterium) and consuming prebiotic-rich foods (fiber, fermented foods) can promote gut health.
Dietary Modifications: A Mediterranean or anti-inflammatory diet rich in polyphenols, omega-3 fatty acids, and fiber can support a healthy gut microbiome.
Stress Management: Mindfulness, yoga, and adequate sleep can help regulate the HPA axis and maintain gut health.
Physical Activity: Regular exercise has been shown to increase microbial diversity and support mental well-being.
Conclusion
The gut-brain connection is a crucial aspect of mental health, with mounting evidence supporting the role of the gut microbiome in mood regulation, stress resilience, and cognitive function. Targeting the gut through dietary and lifestyle interventions offers a promising approach for managing mental health disorders. Future research will continue to uncover the intricate mechanisms linking gut health to psychological well-being.
References
Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior. Nature Reviews Neuroscience, 13(10), 701-712.
Foster, J. A., Rinaman, L., & Cryan, J. F. (2017). Stress & the gut-brain axis: regulation by the microbiome. Neurobiology of Stress, 7, 124-136.
Dash, S., Clarke, G., Berk, M., & Jacka, F. N. (2015). The gut microbiome and diet in psychiatry: focus on depression. Current Opinion in Psychiatry, 28(1), 1-6.
Ma, Q., Xing, C., Long, W., Wang, H., Liu, Q., & Wang, R. (2019). Impact of microbiota on central nervous system and neurological diseases: the gut-brain axis. Journal of Neuroinflammation, 16(1), 53.
Kim, N., Yun, M., Oh, Y. J., & Choi, H. J. (2018). Mind-altering with the gut: Modulation of the gut-brain axis with probiotics. Journal of Microbiology, 56(3), 172-182.
Hi, I’m Jessica, Founder of Finch™ Nutrition.
I’m a California registered dietitian, based in Los Angeles, specializing in digestive health. I offer personalized, judgment-free care to help clients heal from conditions like IBS, Celiac disease, and more—all while honoring their culture, lifestyle, and love for food.
For more info on me and my services, visit www.finchnutrition.com.